The Evidence That IPE Works
In general, I like trials that are LARGE (with thousands of patients), RANDOMISED (comparing a treatment to standard care), BLINDED (so the patient and doctor do not know the treatment allocation), and powered for the most important endpoint—DEATH.
What Is IPE (Icosapent Ethyl – Vascepa)?
It is a combination of fish oils in a tablet that may reduce the risk of heart attack and stroke. It is a branded product with regulated dose content and is thus a medicine rather than a supplement. It is full of EPA and comes in a 1 g tablet.
It is used to lower triglycerides if they are high (>5.64 mmol per litre). High triglycerides can affect the pancreas gland and could lead to elevated cardiovascular risk.
IPE seems to do something useful.
The REDUCE-IT trial was not powered for TOTAL DEATH reduction on its own, which would have made me believe it fully. However, the benefits are hard to argue with, at least in this trial.
The question is why the results of REDUCE-IT were different from the STRENGTH trial when 4g of Omega 3 PUFA (a mix of EPA and DHA) were used. This may be as IPE is more pure EPA, or that perhaps the placebo in REDUCE-IT was having a bad effect! The level of LDL rose slightly in the placebo arm. This is less likely to be the reason.
A further trial of IPE in secondary prevention—so a higher risk group—failed to produce as much benefit:
- It had only 2,500 patients.
- It used 1.8g (not 4g/day).
- It followed patients for only 2 years. Thus, it may have been underpowered to show the effect.
Previous trials have enrolled over 70,000 patients with 1-4 g of EPA/DHA and found very little benefit. In particular, the STRENGTH trial of 13,000 patients showed no obvious benefit versus a corn oil placebo.
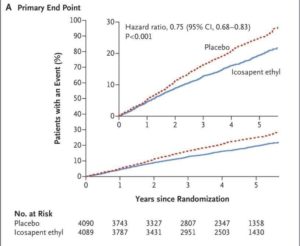
The REDUCE-IT Trial
IPE was used in the REDUCE-IT trial, which suggests it DOES have benefits. They followed patients for about five years.
What Was the Intervention?
They gave 2 g twice a day of IPE to patients with LDL cholesterol, an average of 1.9 mmol/l, stable statin dosing, and triglycerides (TG) > 1.52 mmol/l, later raised to > 2.25 as the trial progressed. The trial aimed to reduce cardiovascular risk, not just triglycerides. They had a run-in period on medication to ensure they could tolerate the IPE.
What Were the Results?
In all comers:
- It reduced the Primary 5-point endpoint by 4.8% absolute risk reduction (ARR) at five years (from 22% placebo vs 17.2% in the IPE group, relative risk reduction 25%).
- The number of patients needed to treat (NNT) to save one endpoint = 21.
- The 3-point endpoint was reduced by 3.6% ARR, NNT = 28.
But:
- There was an increase in hospital admissions due to atrial fibrillation (AF) by 1%.
- An increase in bleeding by 1.9%.
- The IPE was not stopped any more often in the IPE treatment arm versus the placebo arm. BUT remember the run in period? So they had tested that you could tolerate IPE before the start of the trial
This is a chart with IPE showing benefit (blue line)
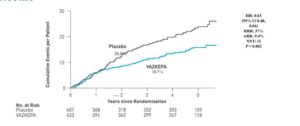
Recent acute coronary syndrome (ACS within 12 months).
In REDUCE-IT this made up about 10% of the trial population:
Primary endpoint 9.3% ARR (28% placebo vs 18.7% IPE, relative risk reduction 37%), NNT=11. There was no more increase in bleeding than the whole group, despite these patients often being on two anti-platelet agents.
Thus, in these higher-risk groups, it does seem to have a more powerful effect on absolute risk reduction and a similar impact on relative risk reduction. Strangely, the effect appears to take over 12 months to start occurring—that is when the curves separate; see below. I would have expected them to begin separating immediately.
Chart showing IPE gives benefit (blue line)
Other subgroups
When looking at patients who appear to be at higher risk, such as diabetic patients or those with established renal disease or peripheral vascular disease, the benefits seem to be maintained. In smokers, the risk of treatment with IPE appears to be reduced to that of non-smokers in the placebo arm!
You can read about the REDUCE-IT trial here.
Conclusion
While IPE shows promise in reducing cardiovascular risk, particularly for high-risk patients, dietary sources of Omega-3s remain an effective and natural way to maintain heart health. If you’re considering supplements, weigh the potential benefits against the risks and consult a medical professional for personalised advice.
Sources: Omega-3 fatty acids for cardiovascular event lowering
Article by Dr Malik, a leading UK cardiologist. He works at One Welbeck Heart Health – London’s Largest Private Cardiology Group, and at Hammersmith Hospital, Imperial College Healthcare NHS Trust, London, one of the largest NHS Trusts in the UK.