This blog post will explore the link between patent foramen ovale and stroke, how it’s diagnosed, and available treatment options. A PFO is a small flap in the heart that doesn’t close after birth. While harmless for most, it can sometimes allow blood clots to bypass the lungs and reach the brain, potentially causing a stroke—especially in cases where no clear cause of stroke is identified, often in younger individuals.
How Does PFO Cause Stroke?
A patent foramen ovale (PFO) can contribute to a stroke through a process called paradoxical embolism. In most people, blood flows from the veins to the lungs, where it is filtered before circulating to the rest of the body. However, in someone with a PFO, a small blood clot or air bubble can bypass the lungs and travel directly from the right side of the heart to the left and then to the brain. This is known as right-to-left shunting and is a key mechanism linking patent foramen ovale and stroke.
Certain factors, such as an atrial septal aneurysm (ASA), can influence how PFO cause stroke. An ASA is a bulging or floppy wall between the heart’s upper chambers, not actually an “aneurysm”. When a PFO and ASA are present together, the risk of blood clots passing through the PFO and reaching the brain is significantly higher.
The size of the shunt varies and it is graded from 0 (no shunt) to 4 (there is so much shunting that bubbles fill the whole of the left side of the heart).
Other risk factors may include situations that raise pressure in the right side of the heart, such as straining during activities like coughing, sneezing, or heavy lifting. These events can temporarily force blood through the PFO, increasing the likelihood of paradoxical embolism.
While most people with a PFO experience no symptoms, some may have signs such as migraines, shortness of breath, or unexplained fatigue, which could indicate the need for further evaluation. You can learn more about PFO symptoms in our blog.
Contact us for a consultation with Dr. Iqbal Malik
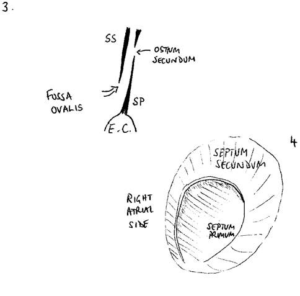
Below, you can see a diagram of the PFO flap in cross-section and from the right side:
PFO Closure and Stroke Prevention
Closing a PFO can be an effective treatment option for lowering the connection between patent foramen ovale and stroke, particularly in individuals who have experienced a stroke with no clear cause (often called a cryptogenic stroke). The procedure involves using a catheter to place a small device that seals the flap in the heart, preventing blood clots or air bubbles from passing through.
Key benefits of the PFO closure procedure include the following:
- Lower Stroke Risk (the main indication)
- Minimally Invasive (compared to one surgery)
- Symptom Relief (rarely)
Book an appointment for PFO closure
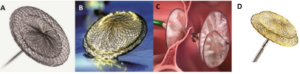
Below, you can see examples of different device options for a PFO closure procedure:
A: Abbott Amplatzer Talismen device
B: Occlutech Figulla Device
C: Gore Cardioform
D: Lifetech Ceraflex device
PFO Closure Stroke Guidelines
Major UK organisations, including the National Institute for Health and Care Excellence (NICE), provide clear PFO closure stroke guidelines:
- Eligibility Criteria: PFO closure is typically recommended for individuals aged 18–65 who have experienced a cryptogenic stroke and have no other identifiable cause, particularly if there is evidence of right-to-left shunting or an associated atrial septal aneurysm.
- Patient Assessment: Comprehensive testing, such as bubble contrast echocardiography, is advised to confirm the presence and severity of the PFO before recommending closure.
- Alternative Options: For patients not suitable for closure, long-term medical management with antiplatelet or anticoagulant therapy may be suggested based on individual stroke risk factors.
These recommendations are personalised to ensure the procedure offers the most benefit to patients at higher risk while avoiding unnecessary interventions for those with lower stroke recurrence risk.
Summary of Patent Foramen Ovale and Stroke
A patent foramen ovale (PFO) is a small opening in the heart that can increase the risk of stroke by allowing blood clots or air bubbles to bypass the lungs and travel to the brain. This connection between patent foramen ovale and stroke is particularly significant in cryptogenic strokes, especially when other risk factors are present. While not everyone with a PFO requires treatment, PFO closure can be an effective option for reducing stroke recurrence in selected patients. Understanding this link helps patients and clinicians explore prevention and treatment options.
Frequently Asked Questions
What are the risks of living with PFO?
Most people with a PFO live without any symptoms or complications. However, in some cases, a PFO can increase the risk of stroke by allowing blood clots or air bubbles to bypass the lungs and reach the brain. Additionally, it has been linked to other cerebrovascular issues, such as transient ischaemic attacks (TIAs). The PFO and stroke risks vary from person to person and often depend on different factors, such as the presence of an atrial septal aneurysm or a history of cryptogenic stroke.
Is there another approach to patent foramen ovale and stroke treatment?
Yes, pharmacological treatment with antiplatelet or anticoagulant medications is an alternative to PFO closure. This approach is often preferred for patients with lower stroke recurrence risk or those who may not be suitable candidates for the PFO closure procedure. The choice depends on individual factors, such as overall health, PFO and stroke history.
You may well have a “belt and braces” approach and continue medical therapy even after PFO closure.
Article by Dr Malik, a leading UK cardiologist. He works at One Welbeck Heart Health – London’s Largest Private Cardiology Group, and at Hammersmith Hospital, Imperial College Healthcare NHS Trust, London, one of the largest NHS Trusts in the UK.